Insulin is one of the most important hormones in the human body, yet it’s a hormone most people don’t really understand. Registered dietitian Linia Patel gives her perspective and advice.
Insulin is produced in the pancreas by the islets of Langerhans and it regulates the amount of glucose in the blood by allowing your body to use glucose for energy or to store glucose for future use. Glucose is a simple sugar that provides the body with its primary source of energy. Glucose in the body comes from digesting carbohydrates (such as rice, pasta, grains or vegetables and fruit). Glucose is carried to the cells through the bloodstream. The human body needs blood glucose (blood sugar) maintained in a very narrow range. In Europe, blood sugar is measured using millimoles per litre. A ‘normal’ blood glucose level comes in at around 4-7mmol/L.
Insulin secretion
Insulin’s main job is to signal to the liver, muscles and fat tissues to take up glucose from the blood and store it as glycogen (the body’s carbohydrate store). As soon as the glucose level in the blood drops to normal, insulin release slows or stops. Although there is always a low level of insulin secreted by the pancreas, the amount secreted into the blood increases as the blood glucose level in the blood rises. Similarly, as blood glucose falls, the amount of insulin secreted by the pancreas goes down. If the blood drops down too low (such as between meals and during exercise) an antagonistic hormone called glucagon is released which does the opposite of insulin, stimulating the breakdown of glycogen and release of glucose to push up blood sugar levels. Insulin also regulates how the body uses and stores glucose and, subsequently, fat. Once carbohydrate has been consumed and is digested into glucose, insulin has three options. The first option is to use blood glucose for metabolic energy. However, if your cells do not need fuel and your blood glucose levels rise above 7mmol/L, insulin signals to the liver to begin synthesising glycogen as its second option. The body has limited ability to store glycogen; hence, once glycogen stores are full, insulin triggers its third option, which is the synthesis of fat from the absorbed blood glucose. Insulin also increases the transport of amino acids from the blood into the cells, therefore stimulating protein synthesis.1, 2
Why is insulin so important?
Like all hormones, insulin has an optimal level and important functions. Without enough insulin, blood glucose builds up in the blood and the cells are starved of their energy source. A lack of insulin or an inability to adequately respond to insulin can each lead to the development of the symptoms of diabetes.
Type 1 and 2 diabetes
Type 1 diabetes is an autoimmune disorder usually diagnosed in childhood. In type 1 diabetes, the cells in the pancreas that make insulin get destroyed. Before researchers discovered how to produce insulin, people who suffered from type 1 diabetes were born with a death sentence. The most effective treatment was to put them on a very strict, minimal carbohydrate diet, which would add a couple more years to a person’s life but definitely wouldn’t save them.3 In 1921, Canadian scientists Frederick Banting and Charles Best successfully purified insulin from a dog’s pancreas. Over the next decades, researchers continued to improve insulin. Insulin from cattle and pigs was used for many years to treat diabetes and saved millions of lives, but it wasn’t perfect, as it caused allergic reactions in many patients. In the early 1980s, biotechnology revolutionised insulin synthesis. Today, insulin now comes in many forms, from regular human insulin, which is identical to what the body produces on its own, to rapid and long-acting insulins. Insulin is still the primary therapy used to treat type 1 diabetes. Type 1 diabetics usually inject themselves with different types of insulin three or four times a day. The treatment for type 2 diabetes, however, differs.
Type 2 diabetes usually develops gradually over a number of years. The condition is also referred to as insulin resistance. Depending on their level of insulin resistance, people with type 2 diabetes may also need to take insulin injections to manage their blood sugar level; however, it can also be managed with a good diet and a healthy lifestyle4.
Insulin resistance: The hallmark of metabolic syndrome
Eating the wrong type or too much carbohydrate will lead to large amounts of insulin being secreted. Continual elevation of insulin leads to large amounts of fat gain (deposited centrally). The more fat tissue you have, the harder it is for your body to use insulin, which ultimately leads to insulin resistance. Insulin resistance is a condition in which the cells of the body become resistant to the hormone. It is also now recognised as a strong predictor of disease in adults. For example, it precedes the development of type 2 diabetes and is associated with an increase of developing heart disease, as well as other medical conditions such as fatty liver and reproductive abnormalities. Interestingly, some recent evidence suggests that whatever organ becomes insulin resistant ends up manifesting its own chronic metabolic disease. For example, if you have insulin resistance of the brain, you end up with Alzheimer’s disease.5
Keeping sensitive
You need insulin but the trick is to learn how to balance the fat storage effects against the anabolic effects in muscle tissue. This can be done by increasing insulin sensitivity in the muscle, while decreasing insulin sensitivity in the fat cells. Controlling the insulin releases during the day is important for long-term sensitivity.
What keeps insulin sensitivity high?
-
The effect of diet
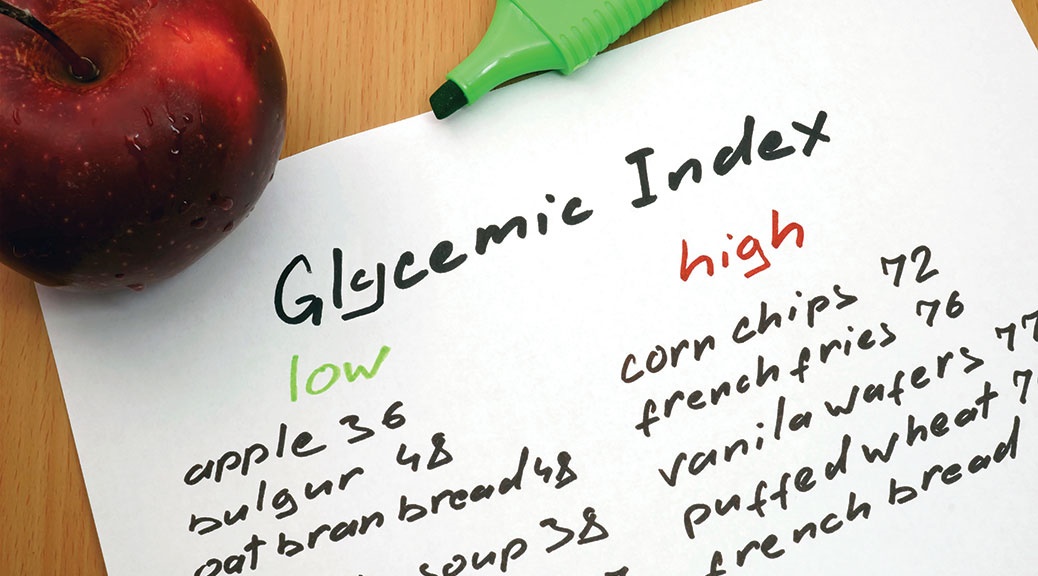
There is a strong body of evidence that shows choosing carbohydrate-dense foods that are low on the glycaemic index may also have beneficial effects, especially when combined with a reduction in calories and regular exercise. It has also been postulated that a plant-based diet containing significant levels of phytochemicals may effectively prevent insulin resistance.6, 7
Research also indicates that a diet high in total (>40% total energy) trans and saturated fat may promote insulin resistance. Replacing saturated fat with polyunsaturated (particularly omega-3 fats) or monounsaturated fat may improve insulin sensitivity, but only if total fat intake also is controlled6. There is currently some evidence that getting enough vitamin D may reduce one’s risk of developing insulin resistance. A recent trial involved 2,000 adults at high risk of type 2 diabetes being either given 2,000 IU of vitamin D per day or a placebo. They found that vitamin D supplementation significantly improved insulin sensitivity and therefore helped control the rise of blood sugar in comparison with the placebo group. While there is a large body of evidence, there is a need to do a large intervention study to fully understand the role of vitamin D and the action of insulin8.
2. The effect of exercise
There is substantial evidence showing improved insulin sensitivity after exercise, both with and independent of weight loss. There’s debate about the best exercise prescription to maximise insulin sensitivity in different populations; both regular aerobic exercise and resistance training seem to confer beneficial results.
A landmark study by Defrenzo et al showed that a simple exercise intervention like walking had a significant impact on insulin sensitivity. In this study, the intervention group participated in a walking programme, although participants were gradually (at the end of four weeks) exercising at a relatively high level of intensity (80-85% of maximum heart rate) for 50-60 minutes per day, five days a week. Level of fitness, as measured by aerobic capacity, was strongly correlated with insulin sensitivity in this study group.9 A randomised 12-week trial designed to examine the effect of exercise (aerobic and resistance) or exercise combined with moderate caloric restriction on insulin resistance showed interesting results. Despite a greater rate of weight loss in the caloric restriction and exercise group (7.4% of initial bodyweight), this didn’t lead to any greater improvement in insulin resistance. A reason for this may be the increased loss of lean muscle mass.10
The importance of sleep
Research has also shown that sleep deprivation and insulin resistance may be linked. A study comparing the impact of sleep deprivation or a high-fat diet on insulin resistance yielded interesting results. The researchers found that the night of sleep deprivation decreased insulin sensitivity by 33%, while six months of a high-fat diet decreased it by 21%.11
10 tips to improve
1. If you are overweight, lose some weight.
2. Exercise for 5 hours a week.
3. Look after your muscle mass.
4. Choose slow-release carbohydrates that are high in fibre
5. Keep your refined carbohydrates in check.
6. Eat a diet rich in monounsaturated fat from sources such as extra virgin olive oil, nuts and avocado.
7. Eat your five-a day or more. Choose a variety of vegetables and fruit that covers a full spectrum of colours.
8. Eat fish frequently. Opt for oily fish, such as wild salmon and sardines.
9. Get sufficient vitamin D – go on a sunny holiday or consider supplementation.
10. Sleep for seven or eight hours per night.
For references, view the Fitpro Magazine references