Dr Arianne Missimer gives us the lowdown on leaky gut.
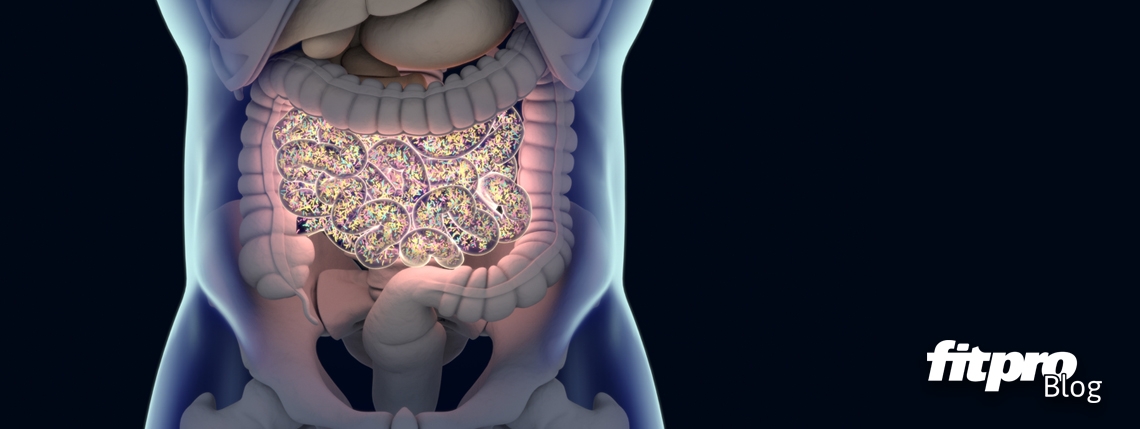
Seventy percent of our immune system lies in our enteric nervous system (ENS), which is located in and around our gut. The ENS defends against illnesses and helps control emotions, appetite and other essential expressions. This intestinal barrier covers a surface of about 400m2, working hard to integrate antigens, specific molecules and nutrients into the body while preventing water and electrolyte loss.(1) It also seals in waste and toxins until they can be disposed of.
At least that’s what it is supposed to do. In the case of intestinal permeability, often called ‘leaky gut’, that protective sheath fails – sometimes alarmingly.
While standard medicine still contests the idea of leaky gut syndrome, continuing research is increasingly connecting it to a whole host of undesirable conditions. A large body of evidence already shows that the gut microbiota’s support of the gut barrier – more specifically, the epithelial barrier – is critical in preventing autoimmune diseases.
What is leaky gut?
When you have intestinal permeability, the pores in your small intestine increase in size, allowing undigested food to enter the bloodstream. This triggers your immune system to attack those particles. At face value, that’s exactly what it’s supposed to do. Unfortunately, it also overcompensates by building up additional, unnecessary antibodies that then have nothing to do but attack healthy cells.
This can lead to a wide range of problems, from allergies to autoimmune diseases, including gastric ulcers, infectious diarrhoea, respiratory infections, arthritis, certain kinds of cancer …(2) The list goes on.
This can all stem from gut microbiota modifications, mucus layer alterations and epithelial damage due to alcohol consumption, energy-dense Western-style diets,(3) exposure to radiation and chemotherapy, and the use of nonsteroidal anti-inflammatory drugs.(4, 5)
How to treat it
Because the negative ramifications of intestinal permeability have not yet been universally accepted, there isn’t always a specific treatment plan or protocol in place. There are, however, strategies available.
According to the Institute of Functional Medicine, the best way to address leaky gut is through a four Rs treatment plan: (6)
- Remove inflammatory foods, medicines, toxins and infections such as candida and SIBO (small intestinal bacterial overgrowth).
- Replace digestive enzymes for proper digestion or break down of foods small enough to allow for proper absorption and use of nutrients for energy, growth and repair.
- Re-inoculate with good bacteria such as prebiotics, probiotics, and fermented food.
- Repair the gut lining with supplements such as L-glutamine, zinc, quercetin and B complex
Although further research clearly needs to be done on the subject to convince the larger medical community, leaky gut sufferers are seeing improvements through nutritional changes. If you think you’re one of them, find a functional medicine or naturopathic doctor who can help you with the proper diagnosis and treatment.
About Dr Arianne Missimer

Dr Arianne Missimer, doctor of physical therapy, registered dietitian, and human movement specialist, has spent the past 18 years in the fitness and nutrition industry. Find out more about Dr Missimer here.
References
1. Bischoff, S.C., Barbara, G., Buurman, W. et al. Intestinal permeability – a new target for disease prevention and therapy. BMC Gastroenterol (2014) 14: 189. https://doi.org/10.1186/s12876-014-0189-7
2. Arrieta, M. C., Bistritz, L., & Meddings, J. B. (2006). Alterations in intestinal permeability. Gut, 55(10), 1512–1520. http://doi.org/10.1136/gut.2005.085373
3. Pendylaya S et al. A High-Fat Diet Is Associated With Endotoxemia That Originates From the Gut. Gastroenterology (2012), 142(5), 1100–1101.e2. http://doi.org/10.1053/j.gastro.2012.01.034
4. Russo F, Linsalata M, Clemente C, et al. The effects of fluorouracil, epirubicin, and cyclophosphamide (FEC60) on the intestinal barrier function and gut peptides in breast cancer patients: an observational study. BMC Cancer. 2013 Feb 4;13:56.
5. Groschwitz, K. R., & Hogan, S. P. (2009). Intestinal Barrier Function: Molecular Regulation and Disease Pathogenesis. The Journal of Allergy and Clinical Immunology, 124(1), 3–22. http://doi.org/10.1016/j.jaci.2009.05.038
6. Institute of Functional Medicine
Where to next? Is there a place in the fitness industry for the neurotrainer?