Associate professor Tom Wainwright and patient Kevin Hubble share ideas for rehabilitation following hip replacement, based on Kevin’s experience as a patient and background as a personal trainer
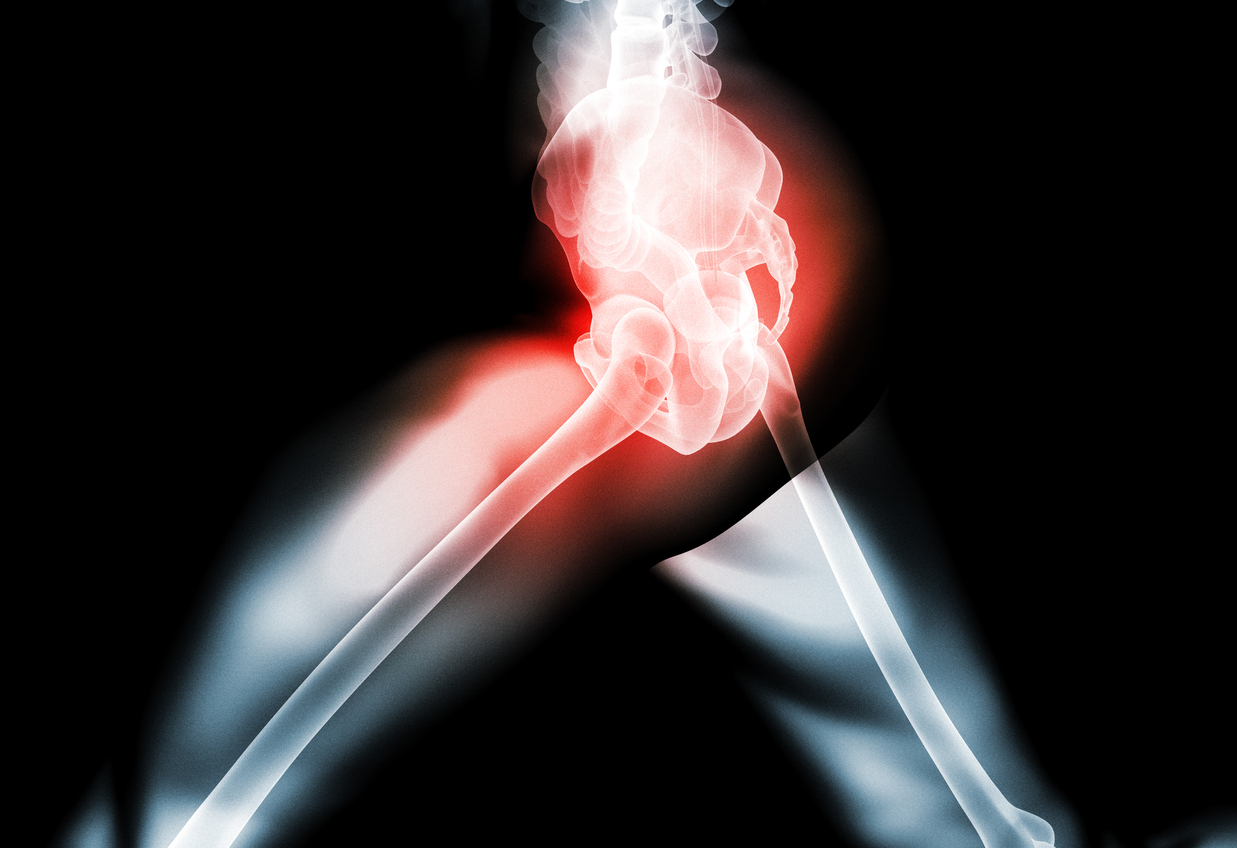
In England, 10.9% of people aged over 45 have osteoarthritis of the hip. This equates to around 2.46 million people, of whom 726,000 have severe symptoms1. Total hip replacement, also termed total hip arthroplasty, is the treatment for end-stage hip arthritis, whereby the hip joint is replaced with an artificial prosthesis2. In 2019, 95,677 hip replacements were performed in the UK3. The majority of surgeries (90%) were performed for arthritis, with the remaining 10% due to hip fracture, avascular necrosis, congenital dislocation, inflammatory arthroplasty or metastatic cancer3. Patients were, on average, aged 69 years, with an average BMI of 28.8 (overweight), and 60% of all patients were female3. With over-65s the most frequent gym users in the UK4, it can be predicted that many of these patients will be members of a gym or leisure centre. Hence, it is likely that many will seek advice from personal trainers on their rehabilitation and return to exercise.
Since the first prosthetic hip was developed in 1938, hip replacement surgery has seen significant change5. Early endeavours were largely limited by poor designs, inferior materials and mechanical failure6. Today, hip replacement surgery is widely recognised as a very successful operation in terms of clinical outcome and cost effectiveness6, 7. As a result, fulfilment of patient expectations has become an increasingly important metric to measure the success of the operation8. For example, in addition to improvements in their pain and functional limitations, younger patients may only be satisfied once they are able to return to employment and participate in sporting activities. To achieve this, and to ensure functional limitations do not develop and persist, effective rehabilitation is paramount9.
Nonetheless, optimal rehabilitation for hip replacement surgery is not well defined10 and many patients experience insecurity regarding how to safely exercise and return to activities of daily living post-operatively11. Current guidelines from the National Institute for Health and Care Excellence (NICE) recommend that acute post-operative inpatient rehabilitation should include mobilisation, advice on managing activities of daily living and a home exercise programme12. However, there are currently no recommendations for longer-term care once the patient is discharged home. Supervised physiotherapy is not regularly prescribed on the NHS and even less so now in the era of COVID-19. As a result, many patients are required to self-manage their rehabilitation once returning home. However, insufficient patient education and low-quality patient information leaflets can impede recovery, as patients avoid exercise due to fear of causing harm, slowing down the rehabilitation process11, 13. Research suggests that many patients do not return to their pre-surgery levels of physical activity at 12 or 24 months following their operation, despite having the physical capability to do so14. Access to education on the levels of exercise suitable for patients following joint replacement is reported as a key barrier to physical activity participation after surgery15. Hence, private practitioners, exercise specialists and personal trainers are well placed to provide advice to patients on how to safely return to exercise and activities of daily living. This article describes the rehabilitation pathway of a typical patient recovering from total hip replacement surgery and provides principles to consider when prescribing exercise for this patient group.
Acute recovery from hip replacement
Immediately following surgery (within 24 hours), patients walk on their new joint and are typically offered advice from a physiotherapist on how to progress mobilisation and how to manage activities of daily living12. In the acute phase of recovery (post-operative days one to three), the aim is to begin to restore functional independence, promote adherence to hip precautions (if used by their hospital) while performing activities, and increase independence with a home exercise programme16. Progressive ambulation with an assistive device (such as crutches) will be encouraged. Commonly prescribed exercises may include: ankle pumps; isometric quadriceps and gluteal holds; hip flexion at 45⁰in supine; sitting knee extension, hip flexion (<90⁰) and standing hip extension, hip abduction and knee flexion16. Precautions vary between surgeon and surgical approach, but may often include avoiding hip flexion past 90⁰, avoiding internal rotation and avoiding hip abduction/adduction past midline for when a posterior surgical approach is used, and avoiding full hip extension and full external rotation when an anterior surgical approach is used17.
A patient will normally be discharged when they are able to safely walk with crutches or walking sticks, safely stair climb, and get on and off a bed, chair and toilet independently, in combination with other factors related to wound healing, X-rays and controlled pain. This is usually one to three days following surgery. If the patient shows difficulties managing their activities of daily living or has ongoing functional impairment, NICE guidelines recommend referral to supervised group or individual rehabilitation12. Otherwise, the patient is provided with a home-exercise programme and advice on self-directed rehabilitation before being discharged home.
From discharge to six weeks
The second phase of physical therapy (discharge to six weeks) focuses on the promotion of wound healing, monitoring pain levels, gradually improving range of motion and strength, restoring normal gait pattern and incorporating functional activities, while adhering to hip precautions12. A home rehabilitation programme may typically include therapeutic exercises to target strength deficits, gait training, proprioception or balance training, cryotherapy, hydrotherapy, functional exercise and promotion of activities of daily living. Initially, pain and oedema may limit movement; however, levels should steadily decline as healing progresses and mobility improves. The patient will normally be reviewed by their surgeon at six weeks post-surgery and, if no signs of complication, they will be encouraged to increase activity levels.
Six weeks to six months
Following the initial six-week recovery phase, it is around this time that patients who are unsure of how to independently manage their recovery may seek advice from exercise specialists and personal trainers. Younger patients who are eager to return to sport or employment may contact a personal trainer earlier. For all patients, it is important that the exercises prescribed are in adherence to any surgeon-specific rehabilitation guidelines. In addition, the patient should demonstrate functional stability and painless movement patterns of the affected joint before a strength and conditioning programme is initiated18. Due to the invasive nature of the surgery, the various approaches to surgery and individual responses to recovery, exercise prescription should be highly individualised. Moreover, patient age, functional ability and comorbidity are strongly associated with rehabilitation outcome19, thus the need for a comprehensive assessment using a tool such as the Physical Activity Readiness Questionnaire (PAR-Q) is recommended:
- age
- weight
- date of surgery
- surgical approach (e.g., anterior or posterior)
- length of stay in hospital
- complications experienced (e.g., post-operative nausea and vomiting, fluid retention, deep vein thrombosis, pulmonary embolism or infection)
- comorbidities
- medication
- functional limitations
- rehabilitation undertaken since surgery
- prior exercise and sporting experience
- goals for rehabilitation.
Exercise prescription following hip replacement
Functional movement training
Initially, exercises should aim to address reductions in the client’s mobility and range of motion that may occur as a result of adaptive tissue shortening pre-operatively, and also during the initial phase of recovery post-surgery16. Exercises performed during the acute phases of recovery can be progressed. For example, lying and standing range of motion exercises can be progressed with equipment such as the TRX, so that an increased range of movement is achieved (see video one). Balance and proprioception exercise prescribed in the initial phases of recovery can also start to be further progressed at this stage. For example, standing and balance exercises could be performed without support, or the client could progress to unstable surfaces or multiplanar movements. Once the client has demonstrated success performing single-plane exercises, they can be progressed to more multidirectional, dynamic movements that progressively load the hip joint (see video two). Load can be progressed and regressed depending on the client’s ability by not only increasing repetitions but also by changing stride length and degree of support offered by the TRX straps.
Cardiovascular conditioning
As rehabilitation progresses, cardiovascular conditioning should be added. Such conditioning can be achieved by creating exercise circuits of the functional movement exercises described previously, but can also be achieved through low-impact exercise. Aerobic exercise that combines cyclic lower-limb movement patterns with minimal rotational and impact forces (e.g., cycling, swimming and walking) are recommended to improve cardiovascular conditioning. While vigorous activity should be carefully introduced in the first three to six months post-operation, moderate-exercise intensity is needed to enhance cardiovascular benefits. Guidelines from the National Strength and Conditioning Association suggest initiating aerobic exercise at a light-to-moderate intensity (55% to <75% of the client’s maximal heart rate [MHR] or a rate of perceived exertion [RPE] of 9-13 on the Borg scale), and progressing to a moderate (65% to 75% MHR/RPE 12-13) and high intensity (≥75% MHR/RPE ≥14) when suitable18. Therefore, utilising heart-rate monitoring equipment (such as a MYZONE or equivalent) can be extremely useful to regulate effort and increase/decrease intensity based on reaction to activities. High-impact activities, frequent jumping and contact sports should be limited in the early stages of rehabilitation.
Loaded functional movement training
To induce hypertrophy and strengthening, muscles and connective tissues must be subjected to a load greater than their usual stresses20. Therefore, adding load to functional movement patterns can elicit these adaptive responses; however, rehabilitation intensity must be managed in accordance with the healing stage of tissues to avoid reactive inflammation20. Therefore, it is suggested that resistance training begins with a relatively low weight and higher repetitions (one set of eight and 12 repetitions) to improve muscular endurance while accommodating the fragility of healing tissue. As rehabilitation progresses, an increase in exercise intensity (with increased load) can induce strength gains. Guidelines from the National Strength and Conditioning Association recommend beginning with one session of resistance training per week and progressing to two sessions per week as tolerated by the client18. It is largely agreed that prescribing exercises that replicate functional movement patterns will help the client to complete activities of daily living. Initial considerations for the implementation of a functional programme should revolve around the physical parameters of the client’s intended recovery (e.g., returning to work, driving or a sporting activity). Some ideas for exercises that can be used, which incorporate an increase in load but build on the movement and proprioceptive challenges of the exercises demonstrated earlier, can be found in video three.
How I recovered from a hip replacement
Kevin Hubble had a hip replacement in 2019. He shares his personal reflections on his recovery and rehabilitation.
 I found that, even with years of experience in the fitness industry and my understanding of biomechanics, I was initially unsure of and unrealistic about how I was going to manage my rehabilitation. I wanted to get back to full recovery and being able to squat, shuffle and jump as soon as possible, but I soon came to realise that it was going to be a gradual process and I had to really put some thought into how I was going to achieve this, because even the simple things like walking without a limp were a problem initially after my operation.
I found that, even with years of experience in the fitness industry and my understanding of biomechanics, I was initially unsure of and unrealistic about how I was going to manage my rehabilitation. I wanted to get back to full recovery and being able to squat, shuffle and jump as soon as possible, but I soon came to realise that it was going to be a gradual process and I had to really put some thought into how I was going to achieve this, because even the simple things like walking without a limp were a problem initially after my operation.
So, I put my ‘biomechanical head’ on and planned my rehab properly. My first port of call was trying to get range of motion in simple things like squatting, so that I could sit on a chair without cheating to get up, and also being able to stand on one leg. My reasoning for this was that, while walking, as one leg leaves the floor, the other must support you. With that in mind, and with the aim of losing my limp, I came up with an initial programme. I worked on gluteal strength and range of motion at the beginning, in conjunction with using the swimming pool for mobility and resistance. I spent a lot of my time using the TRX suspension trainer, as I needed to learn to set the standard again with exercises, and worked on foundation movements.
As you will see in the exercise videos, during the later rehab process a lot of my exercises involved working in three planes of motion and, as time went on, I increased my range of movement to increase the load but I never went too far with it. Knowing your limits and working gradually is very important. As my rehabilitation progressed, I started to use ViPR so that I could change the weight distribution and, therefore, the load on my hip. It helped me to build in more dynamic movements and shuffles, so that I could achieve my later stage rehabilitation goals.
Fancy learning more about joint replacements and how to work with clients? Check out our online education Training Clients with Joint Replacements
Authors
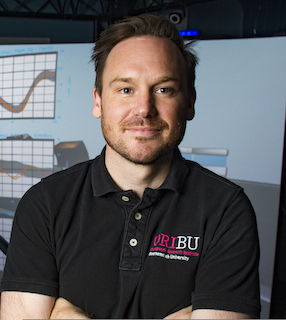
Tom Wainwright is a physiotherapist and Associate Professor in Orthopaedics at the Orthopaedic Research Institute, Bournemouth University. He is internationally recognised for his work on Enhanced Recovery after Surgery protocols, and he has active research projects related to osteoarthritis, orthopaedic surgery, and rehabilitation.

Louise Burgess, who assisted with writing the article, is a research assistant at Bournemouth University.
This article originally featured in the Fitpro digital magazine.
References
- Versus Arthritis. State of musculoskeletal health 2019. 2020 Available from https://www.versusarthritis.org/about-arthritis/data-and-statistics/state-of-musculoskeletal-health-2019/, accessed on 29 October 2020.
- Siopack JS, Jergesen HE (1995), Total hip arthroplasty, West J Med., 162(3): 243-9.
- National Joint Registry (2020), National Joint Registry 17th Annual Report 2020. Available from https://reports.njrcentre.org.uk/Downloads, accessed on 29 October 2020.
- Nuffield Health (2016), Rise of the active over 65s: Figures show those aged 72 are UK’s most regular gym users. Available from https://www.nuffieldhealth.com/article/rise-of-the-active-over-65s-figures-show-those-aged-72-are-uks-most-regular-gym-users, accessed on 29 October 2020.
- Wiles P (1958), The surgery of the osteoarthritic hip, Br J Surg., 45(193): 488-97.
- Learmonth ID, Young C, Rorabeck C (2007), The operation of the century: total hip replacement, Lancet, 370(9597): 1,508-19.
- Konopka JF, Lee YY, Su EP, McLawhorn AS (2018), Quality-Adjusted life years after hip and knee arthroplasty: health-related quality of life after 12,782 joint replacements, JB JS Open Access, 3(3): e0007.
- Kahlenberg CA, Nwachukwu BU, Schairer WW, Steinhaus ME, Cross MB (2017), Patient satisfaction reporting after total hip arthroplasty: A systematic review, Orthopedics, 40(3): e400-e4.
- Okoro T, Lemmey AB, Maddison P, Andrew JG (2012), An appraisal of rehabilitation regimes used for improving functional outcome after total hip replacement surgery, Sports Med Arthrosc Rehabil Ther Technol., 4(1): 5.
- Bandholm T, Wainwright TW, Kehlet H (2018), Rehabilitation strategies for optimisation of functional recovery after major joint replacement, J Exp Orthop., 5(1): 44.
- Jappinen AM, Munoz M, Kettunen T, Piirainen A (2020), Patients’ narratives of patient education in physiotherapy after total hip arthroplasty, Physiother Res Int., 25(4): e1862.
- National Institute of Health and Care Excellence (2020), NICE guideline [NG157] Joint replacement (primary): hip, knee and shoulder. Available from https://www.nice.org.uk/guidance/ng157, accessed on 29 October 2020.
- Wainwright TW, Burgess LC (2018), To what extent do current total hip and knee replacement patient information resources adhere to enhanced recovery after surgery principles?, Physiotherapy, 104(3): 327-37.
- Smith TO, Mansfield M, Dainty J, Hilton G, Mann CJV, Sackley CM (2018), Does physical activity change following hip and knee replacement? Matched case-control study evaluating Physical Activity Scale for the Elderly data from the Osteoarthritis Initiative, Physiotherapy, 104(1): 80-90.
- Smith TO, Latham S, Maskrey V, Blyth A (2015), Patients’ perceptions of physical activity before and after joint replacement: a systematic review with meta-ethnographic analysis, Postgrad Med J,. 91(1079): 483-91.
- Cioppa-Mosca JCJBC, Corradi-Scalise JT, Rudnick D, Wolff H (2006), Total Hip Arthroplasty Postsurgical RehabilitationGguidelines for the Orthopaedic Clinician, Missouri Mosby Elsevier, 4-16.
- Madara KC, Marmon A, Aljehani M, Hunter-Giordano A, Zeni J, Jr., Raisis L (2019), Progressive rehabilitation after total hip arthroplasty: A pilot and feasibility study, Int J Sports Phys Ther., 14(4): 564-81.
- National Strength & Conditioning Association (NSCA), Jacobs P (2017), Understanding and Recommending the Exercise for Clients with Joint Replacements. NSCA’S Essentials of Training Special Population, Human Kinetics.
- Snell D, Hipango J, Sinnott KA, Dunn JA, Rothwell A, Hsieh CJ et al (2018), Rehabilitation after total joint replacement: a scoping study, Disabil Rehabil., 40(14): 1,718-31.
- Andrews JRH, Wilk KE (2012), Physical Rehabilitation of the Injured Athlete, 4th edition, Cambridge: Elsevier.