A systematic approach to improving ankle mobility
When called upon, all links in the kinetic chain add to the body’s ability to summate forces for acceleration and dissipate forces for deceleration. Having the optimal motion and mobility at each joint allows the body to utilise the architecture of the joint and the soft-tissue structures to the best of their ability.
Ankle mobility is no different. The effects of limited dorsiflexion can be observed in most upright movements with the foot fixed to the ground during locomotion. Because of the ankle’s proximity to the foot and the ground, its function yields a tremendous influence on the structures above on both the ipsilateral and contralateral sides of the body.
Research has linked limited dorsiflexion to injuries in the lower leg, such as plantar fasciitis, shin splints, stress fractures, ankle sprains and Achilles’ tendinitis. In the knee, limited dorsiflexion is seen in people with patella femoral pain.
Two-legged squatting with limited dorsiflexion increases knee valgus, decreases quadriceps activity and increases soleus activity. In addition, limited dorsiflexion in jump landing has been tied to increased ground reaction forces, reduced knee flexion and increased knee valgus — all of which increase the risk of anterior cruciate ligament (ACL) injury.
Unfortunately, many health and fitness professionals address the challenges of ankle mobility from a very narrow perspective. Improving ankle mobility requires much more than myofascial release of the calves and stretching the calves with the ankle in dorsiflexion in the sagittal plane.
If we consider the bony geometry of the foot and ankle and the continuity of the myofascial tissue at the back of the gastrocnemius and soleus to the metatarsal heads, and cranially with the relationship to the hamstrings, we can see many overlooked opportunities to improve ankle mobility.
The foot and ankle consist of a combined 26 bones that make up 33 joints. By involving the complementary motions of these joints and the associated soft tissues that act on them, we can identify an abundance of ways to develop mobility strategies.
The bones
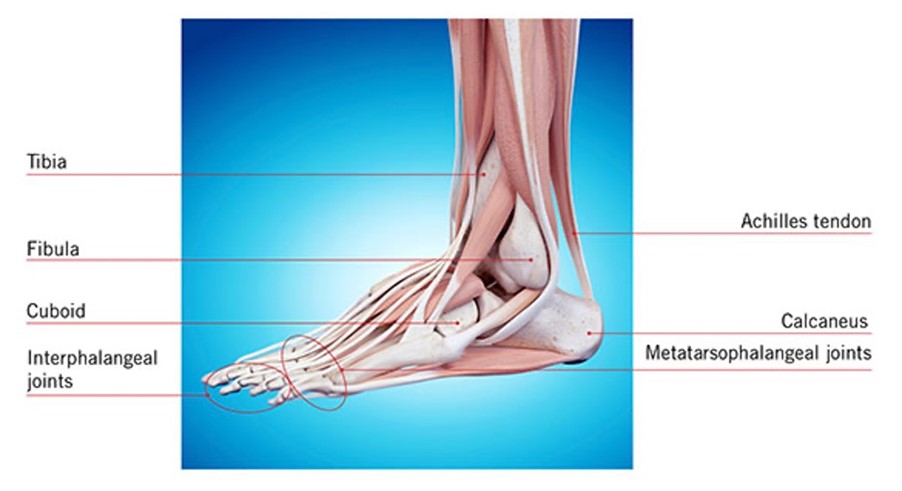
The ‘true’ ankle joint is the talocrural joint. This joint is formed by the talus below and the distal ends of the tibia and fibula, which form a mortise, or archway, for the talus to move under. This is the joint where dorsiflexion occurs and where most would target for enhancing ankle mobility.
The subtalar joint is the joint below the true ankle joint and is made up of the talus sitting in the calcaneus. This is where pronation and supination occur. The Achilles’ tendon wraps around the calcaneus prior to passing to the plantar aspect of the foot and merging with the plantar fascia.
Midtarsal joints are formed by the articulation of the calcaneus with the cuboid and the articulation of the talus with the navicular. This joint creates inversion or eversion of the rear foot relative to the forefoot, which serves to increase or decrease the medial arch. At the toes are the metatarsophalangeal joints and the interphalangeal joints, which allow for toe flexion and extension.
At the knee joint, which the gastrocnemius crosses, the tibiofemoral joint allows for a limited amount of transverse and frontal plane motion, along with the much greater flexion and extension motions.
By understanding the involved joints and their available motions, individually and combined with other joints, it becomes clear that the tissue needs to be lengthened along multiple vectors.
The following is a proposed systematic strategy for addressing ankle mobility, with an appreciation for the multiple joints involved and the multiple directions in which the tissue that crosses the ankle joint works.
Self-myofascial release
As previously mentioned, self-myofascial release can be a valuable aspect of soft-tissue mobility anywhere on the body, including the calves. However, because there is continuous myofascial connection from the plantar fascia to the hamstrings, the foot and posterior thigh should be included as well.
Start with the bottom of the foot, using a small ball or series of small balls of varying sizes and densities. Move from the bottom of the foot to the posterior lower leg using a roller. Use a tennis ball or similarly sized ball to target areas of the lower leg with more specificity. For example, you can target the tissue between the lateral gastrocnemius/soleus and the peroneals.
Work your way up to the hamstrings to include all three muscles by rotating the thigh slightly to address the medial and lateral aspects of this muscle group.
The exact mechanisms behind why self-myofascial release works are still not clear in the literature. However, there are multiple studies that have validated its benefits relating to improved range of motion.
Want to learn more? Check out more education from Anthony Carey and Kevin Murray in their online education Pain-Free Movement Specialist.








